Introduction
Stroke is the leading neurological disease in the world that causes long-term disability (1,2). Worldwide, the incidence of stroke has increased by 70% in the last decade (3). In Europe, more than one million cases are reported each year, and nine million stroke survivors are alive right now (4). The annual estimated cost of stroke treatment in Europe is twenty-seven billion euros, and it is estimated to reach up to 184 billion dollars by 2030 (5). Therefore, it is necessary to develop an economical rehabilitation program that prevents or reduces long-term disability after stroke.
Stroke survivors may experience various problems, depending on the severity, like impaired mobility, balance, function, cognition, and psychological problems. Almost two-thirds of individuals with stroke have impaired mobility and functional limitations resulting from brain damage (6). The quality of life is also disturbed by the abnormal gait patterns of individuals with strokes. Individuals who have had a stroke can walk with capacity, which plays an important role in improving their quality of life. The reduced walking capacity of these patients may limit their social participation. Therefore, impaired walking capacity should be adequately addressed (7). High-intensity exercise resulted in greater improvement in walking speed, stride length, and cadence compared with conventional gait training in chronic stroke patients (8). However, traditional high-intensity training (HIT) may cause increased blood pressure and arterial stiffness (9) and is not feasible for stroke patients with limited mobility. Therefore, a safer, feasible, and cost-effective training program for stroke patients with limited mobility is needed. Blood flow restriction (BFR) with resistance training may be an economic and time-efficient alternative to HIT to manage the risk factors of stroke and can also be useful in reducing stroke-related impairment effectively.
Karatsu training, or BFR, was first introduced as a common exercise in Japan, and some scientists considered it the “state of the art” exercise. During BFR training, the blood flow of the exercising muscle is restricted by placing the inflated tourniquets at the most proximal parts of the legs or arms (10). By restricting the blood flow to the limbs, the desired muscle group will work in an ischemic environment and can trigger a significant increase in hypertrophy/muscle mass, power, and strength (11) by recruiting the fast twitch muscle fibers (12).
Previous evidence from neurological studies has shown that BFR training can improve muscle strength, balance, walking capacity, and cognitive function in multiple sclerosis and incomplete spinal cord injury patients (11,13,14). A recent study showed that BFR training has improved brain-derived neurotrophic factor (BDNF) and vascular endothelial growth factor (VEGF) and the rate of perceived exertion in ischemic stroke patients (14). Similarly, a randomized controlled trial (RCT) reported a significant improvement in upper limb motor recovery and function in the BFR group compared with exercise training alone in stroke patients (15). Recently, it was found that the neurophysiological response of BFR in stroke patients was reported to have no significant difference between BFR and exercise groups after one session (16). Despite its beneficial effects, to the best of our knowledge, no study has investigated the effect of low-intensity resistance training with BFR (LIRT-BFR) on balance, muscle strength, walking capacity, and depression in patients with stroke. It is hypothesized that both LIRT-BFR and HIRT will yield a similar improvement in balance, muscle strength, walking capacity, and depression in patients with ischemic stroke. This RCT will compare the effects of a 5-week LIRT-BFR combined with aerobic training versus a 5-week HIRT combined with aerobic training on balance, muscle strength, walking capacity, and depression in stroke survivors.
Materials and Methods
Study Design and Ethical Approval
It will be a single-blinded, two-arm, parallel RCT, which will be conducted in accordance with the tenets of the Helsinki Declaration. The RCT has been designed according to the SPIRIT (17) and CONSORT (18) guidelines and has been approved by Non-Invasive Clinical Research Board of Istanbul University-Cerrahpasa on 02-02-2022 (protocol no:E-74555795-050.01.04-335759). This trial was prospectively registered at www.clinicaltrials.gov (identifier: NCT05281679). The SPIRIT schedule of study is shown in Figure 1.
The research will be carried out at the outpatient Department of Physiotherapy and Rehabilitation, Faculty of Health Sciences, Istanbul University-Cerrahpasa. Written informed consent was provided by all the stroke survivors included in this study.
Participants and Eligibility Criteria
Patients with more than one month of stroke will be eligible for the study. All the participants will be evaluated to be in stable cardio-vascular condition, i.e., ACSM Class B (19). The inclusion criteria will be: (1) 18 to 75 years of age; (2) more than 1 month of stroke onset; (3) first-ever unilateral ischemic stroke (4) walking 10 meters independently with or without an assistive device; (5) being an independent ambulator (Functional Ambulation category >3); and (6) modified Ashworth scale < grade I. The exclusion criteria were: (1) people with a history of mental/cognitive illness; (2) transient ischemic attack; (3) combination with peripheral neuropathy; (4) having resting blood pressure above 160/100 mmHg even after taking medications; (5) hemorrhagic stroke (6) cardiovascular comorbidity (heart failure, unstable angina, aortic stenosis, arrhythmias, hypertrophic cardio-myopathy, depression of ST-segment); (7) people with obvious cognitive impairments; (8) by-pass surgery in the last 3 months; (9) any musculoskeletal condition that resists or limits the participants from doing resistance training; and (10) people who have taken analgesics, dopamine, antipyretics, and any other drugs that can affect the function of the autonomic nerve system in the last 2 weeks.
Sample Size
Stata version 16.0 was used to determine the sample size by using the reported effect size of the 6-minute walk test (6-MWT) on patients with stroke in a prior study (20). The minimum sample size required to show a clinically significant difference of 55 meters in the 6-MWT [two-tailed type I error of 0.05; power of 90%; standard deviation (SD) of 40] was 13 per group. A total of 32 patients (16 in each group) will be recruited after considering a dropout rate of 20%.
Randomization
Participants will be randomly allocated to LIRT-BFR or HIRT without the BFR group. Microsoft Excel software will be used for the randomization. Specifically, a random number between 0 and 1 will be assigned to each group (distribution to groups was based on: 0 to <0.5 = HIRT group and 0.5 to <1 = LIRT-BFR group). The generated random numbers will be placed in a sealed envelope and kept in a container. An individual, with no other role in the study, will pull a sealed envelope out of a container to decide the distribution of participants. The envelopes will be designed to achieve the allocation of a 1:1 ratio of LIRT-BFR to HIRT groups. Group allocation will be blinded to the assessor to ensure group concealment. After the randomization process, the participants will receive information about the group they are allocated to. Figure 2 shows the distribution of patients.
Training Intervention
After the randomization process, patients in the LIRT-BFR and HIRT groups will undergo five weeks of treatment in the outpatient department. The HIRT group will receive high-load resistance training (40 min, 3 days/week), while the LIRT-BFR group will receive LIRT-BFR (40 min, 3 days/week). The duration of training will be 5 weeks for both groups. In addition to resistance training, all the participants will perform 20 min of aerobic training without BFR (treadmill and cycling training, 10 min each).
Determination of 1-repetition Maximum
During the first visit, the subjects will be familiarized with the use of test instruments and will be screened for one-repetition maximum (1-RM) tests, which are widely used to determine muscular strength and consist of the highest load that can be lifted in a single repetition through a full range of motion (14,21). After two minutes of warm-up, participants will choose, according to the range self-predictability, an initial weight (50-70%) of 1-RM. After each test, a 10-20% weight increment will be added until they reach the final limit (maximum load) that can be lifted once. A 3-5 minute recovery interval will be provided between the two tests, and the maximum weight lifted will be recorded as 1-RM (14).
Low Intensity Resistance Training with the Blood Flow Restriction Group
The LIRT-BFR group will perform three sets of low-load resistance exercises, targeting the large muscles of the legs at 40% of their 1-RM. The resistance training protocol consists of 3 sets of 6 exercises (knee extension, hip flexion, extension and abduction, straight leg raise using a sandbag, leg press, and squat). Each set consisted of 10 repetitions of 1-RM with a 1-min recovery interval between sets and 3 min between exercises. Subsequent 1-RM testing procedures will be performed every week, where the weight load will be readjusted to 40% of 1-RM. Blood flow to the active muscles during LIRT-BFR training is restricted by a BFR band (tourniquet) placed at the proximal end of the lower limbs. When participants perform LIRT-BFR training, the proximal portion of their lower limb was compressed at 150-160 mmHg by a blood pressure cuff (22). The air pressure belt will be inflated before the exercise and will remain inflated during the one-minute intervals between the sets and will be deflated during the three-minute intervals between the exercises.
High-Intensity Resistance Training Without the Blood Flow Restriction Group
The HIRT group will perform 3 sets of high load resistance exercises, targeting the large muscles of the legs at 80% of 1-RM. The resistance training protocol consists of 3 sets of 6 exercises (knee extension, hip flexion, extension, and abduction, straight leg raise using a sandbag, leg press, and squat). Each set consisted of 10 repetitions of 1-RM, with a 1-minute rest interval between sets and a 3-minute rest interval between exercises. Subsequent 1-RM testing procedures will be performed every week, where the weight load will be readjusted to 80% of the 1-RM.
Outcome Measures
The outcome measures will be obtained at baseline and post-intervention (5 weeks). After taking the baseline measurements, participants will be randomized by a therapist not involved in the recruitment, intervention, or assessment process of the study. All the outcome measurements will be obtained from an assessor who will be blinded to the group allocation. Patients will be instructed to avoid mentioning their treatment plan to the assessor. The accessor (physiotherapist) will be trained to ensure consistency in the assessment process and to ensure that the protocol is standardized. All the demographic measurements, location, type of stroke lesion, time post-stroke, and functional ambulation category score to determine the post-stroke functional ability will be collected at baseline. The 10-meter walk test, five-time sit-to-stand test, timed up and go test, 6-MWT, and Barthel index test will be the primary outcome measures. The secondary outcome measures will be anxiety and depression as measured by the hospital anxiety and depression scale, gait speed, stride length, cadence, adherence to treatment intervention, and adverse events. In addition to these outcome measures, blood pressure, heart rate, and oxygen saturation will be monitored daily during the intervention.
Primary Outcome Measures
Five time sit-to-stand test: Five time sit-to-stand test will be used to assess lower extremity muscle strength, balance, and risk of fall in stroke patients (23). The test measures the amount of time taken to complete five repetitions of the sit-to-stand task. The test was performed using a standard-height chair without an armrest and with a straight back (43-45 cm high). The patients will be instructed to, by keeping their arms folded across their chest, stand up and sit down as quickly as possible five times. The stop-watch will be started when the patient’s back leaves the backrest of the chair and stop once the back touches the backrest of the chair for the fifth time (24).
10-meter walk test: The 10-m walk test will be used to determine the gait speed of walking. A 14-meter corridor will be used for the test, and patients will be allowed to use a walking aid if necessary. Patients will be instructed to walk comfortably. The stopwatch will be started at the 2nd meter and stopped when the patient reaches the 12th meter. After three tests, the average of the three tests will be recorded (20).
Timed up-go test: The timed up-go test is a functional mobility test used to assess dynamic balance, transfer, and gait. The patients will be instructed to stand up, with support for the arms, from a chair (46 cm high), walk for a short distance (3 m), turn, go back, and sit down as quickly as possible. The stopwatch will be used to measure the time it takes to perform these tasks from start to finish. The patients will be allowed to use their walking aids (25,26).
6-minute walk test: The walking distance will be measured by the 6-MWT, the most commonly used for measuring the functional exercise capacity of individuals after stroke (27). The patients will be instructed to walk as far as possible throughout the 30-meter course within 6 minutes by following the standardized instructions provided by the physiotherapist. Participants will be allowed by the physiotherapist to use an aiding device if necessary. The physiotherapist will guard the participants during the walk test but will not offer any assistance or support to the participants.
Barthel index (BI): The level of independence in functional activities is determined by the BI. It included ten items, and the score range between 0 and 20 points show complete dependence; between 21 and 61 points, severely dependent; between 62 and 90 points, moderately dependent; between 91 and 99 points, lightly dependent; and 100 points indicate complete independence (20,28).
Secondary Outcome Measures
Anxiety and depression: The hospital anxiety and depression scale, which is the most widely used scale in the clinical evaluation of stroke patients, will be used to measure anxiety and depression (29). It includes anxiety and depression subscales and consists of 14 items, 7 of which investigate depression and 7 of which investigate anxiety symptoms. Responses are evaluated in a four-point Likert format and scored between 0 and 3 (30).
Walking parameters: Walking time and number of steps during 10-meter walk test will be assessed to calculate gait speed (m/s), stride length (cm), and cadence (steps/min). After three trials, the average of the three trials is recorded as m/s (20).
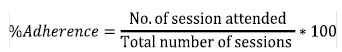
Adherence: Adherence to the intervention program will be calculated as a percentage using the following formula:
Adverse events: Participants will be advised to report any adverse or unexpected symptoms (change in blood pressure, heart rate, pain, etc.) to the physiotherapist. A logbook will be used to document any adverse or unexpected symptoms.
Statistical Analysis
The normality of data will be tested using the Shapiro-Wilk test of normality. The descriptive analysis will be reported as the mean and SD. Baseline data will be collected at T0. Measurements will be repeated after five weeks of intervention (T1). To compare the normally distributed continuous demographic variables, the independent t-test will be used, and for not normally distributed continuous variables, the Mann-Whitney U test will be used. For categorical demographic variables, the chi-square with Yates’ adjustment or Fisher’s exact test will be used. If the data are normally distributed, we will use a parametric test (e.g., Paired samples t-test, Independent Samples t-test), whereas if the data are not normally distributed, we will use a non-parametric test (e.g., Wilcoxon signed-rank test, Mann-Whitney U test). The effect size is determined by Cohen’s d coefficient value and was considered large (0.5), moderate (0.3), and small (0.1) (31). All the data will be analyzed using SPSS version 24.0 (SPSS Inc., Chicago, IL).
Discussion
Although resistance training is commonly used to treat stroke patients, HIRT is not only more intensive but also less safe and suited for long-term use. Högg et al. (32) reported that 26% of stroke patients reported joint pain after HIRT. LIRT-BFR improves muscle strength, balance, walking capacity, and cognitive function in neurological patients. The hypertrophy responses induced by LIRT-BFR are comparable to those produced by HIRT (33). Previous studies have determined the neurophysiological and hormonal response of BFR in stroke patients, and this will be the first RCT to evaluate the effects of LIRT-BFR on balance, lower limb muscle strength, walking capacity, and depression in stroke survivors. Another novel aspect of this study will be that it will not only determine the effect of LIRT-BFR but also compare the improvement achieved with HIRT. The marked expected improvement in lower extremity muscle strength, balance, walking capacity, and depression will allow stroke patients to have a more active lifestyle and will improve their quality of life. The important findings will provide clinicians and physiotherapists with the information they need to modify resistance training in stroke rehabilitation to maximize motor recovery, as well as encourage clinicians and physiotherapists to use BFR during stroke rehabilitation.
Safety and Efficacy
This single-blinded RCT will provide valuable information about the safety and efficacy of BFR therapy in stroke rehabilitation. Previous studies in high-risk groups of patients, such as those with cardiovascular disease, stroke, etc., reported that BFR is safe and produces significant improvement (34). In addition, BFR training and HIT produced a similar effect on both systolic and diastolic blood pressure and heart rate in young individuals and older adults (35).
Study Limitations
This RCT will constitute an evidence-base for BFR training and its efficacy on lower limb strength, walking capacity, and balance performance in stroke patients. Secondly, the randomization is stratified by age and sex variables, which may influence the prognosis. Moreover, the accessor and the person who performs the randomization will be blinded to the group allocation. Finally, the sample size of this study was calculated to detect the minimum clinical difference, which will help detect the differences in outcome measures.
Our research has a few limitations. Although the accessor was blinded to the group allocation, due to training, we could not blind the patients and therapists for treatment allocation. Secondly, we don’t know whether the current range of cuff pressure for BFR is suitable for stroke patients. The cuff pressure used in this study is based on BFR training in sub-acute stroke. Finally, the study will recruit only ischemic stroke patients, and the findings of this study might not apply to patients with hemorrhagic stroke.
Conclusion
Previous studies determined the effect of BFR training in stroke patients and could only report the improvement in BDNF and VEGF levels and could not report any physical function outcome. Therefore, this RCT will assess the effect of BFR with resistance training on physical function outcomes in ischemic stroke patients.
Ethics
Ethics Committee Approval: The ethical approval has been approved by the Non-Invasive Clinical Research Board of Istanbul University-Cerrahpasa on 02-02-2022 (protocol no: E-74555795-050.01.04-335759).
Informed Consent: Written informed consent was provided by all the stroke survivors included in this study.
Peer-reviewed: Internally peer-reviewed.
Authorship Contributions
Concept: I.A., R.M., B.E., Design: I.A., R.M., Data Collection and/or Processing: I.A., R.M., B.E., Analysis and/or Interpretation: I.A., R.M., Literature Research: I.A., Writing: I.A., R.M., B.E.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.